 Bacterial infections can take hold in the body when a pathogenic, or disease-causing, microorganism enters and delivers toxins to healthy human cells. One way bacteria accomplish this is by releasing vesicles, which act as tiny envelopes transporting toxins and other virulence factors―molecules that help infection take hold―to host cells. The virulence factors allow the bacteria to effectively infect healthy human cells and make people sick.
Bacterial infections can take hold in the body when a pathogenic, or disease-causing, microorganism enters and delivers toxins to healthy human cells. One way bacteria accomplish this is by releasing vesicles, which act as tiny envelopes transporting toxins and other virulence factors―molecules that help infection take hold―to host cells. The virulence factors allow the bacteria to effectively infect healthy human cells and make people sick.
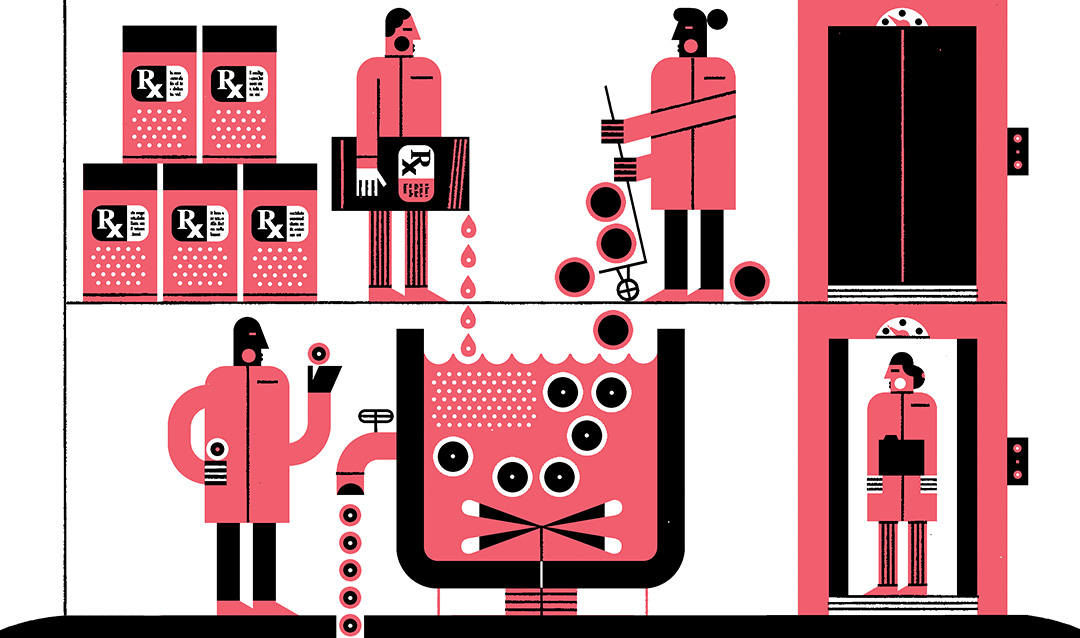
The rapid emergence of antibiotic-resistant bacteria―bacteria that do not respond to currently available antibiotic treatment―is a worldwide problem that is only expected to worsen. The Centers for Disease Control and Prevention (CDC) estimates that almost three million people in the U.S. develop antibiotic-resistant bacterial infections each year, with more than 35,000 dying as a result. Developing new antibiotic drugs is a long and expensive process and not widely seen as an effective long-term solution. Anti-virulence strategies that seek to disarm bacteria’s virulence factors are one possible approach.
“The idea of an anti-virulence strategy is to eliminate those virulence factors or inhibit the function of those so the bacteria don’t have those advantages,” says Angela Brown, an associate professor of chemical and biomolecular engineering whose research has focused on anti-virulence strategies. “Then the immune system could have time to clear the infection before it takes hold.”
Recently, Brown’s research has taken a promising turn. She is now leveraging her extensive knowledge of bacterial vesicles to develop a better drug-delivery system that could help combat antibiotic resistance.
Brown and her team are harnessing the power of outer membrane vesicles―which are continuously shed by Gram-negative bacteria, the most difficult to treat―to deliver drugs directly to cells. Such a system could decrease the rate of resistance by, among other outcomes, improving delivery to bacteria that are particularly difficult to treat with antibiotics, including those that have developed certain resistance traits.
“Bacterial vesicles as a delivery system have a number of advantages,” says Brown. “They are really stable and they have a natural ability to deliver large molecules to other cells.”
Although other researchers have demonstrated the feasibility of using outer membrane vesicles to deliver medicines, the method has its limitations. Brown’s team is working on a way to overcome those limitations by combining the best properties of outer membrane vesicles with another promising drug delivery strategy: liposomes. Liposomes are synthetically created, nanometer-scale, spherical vesicles that are attractive as drug delivery vehicles because of their solubility and low toxicity. Liposomes’ stability, however, is limited.
“We want to combine liposomes and outer membrane vesicles to create ‘semi-synthetic outer membrane vesicles,’” says Brown. “This will result in a delivery system that maintains the advantages of each system while overcoming the limitations of each.”
Read the full article in the 2021 Lehigh Research Review.
Story by Lori Friedman

