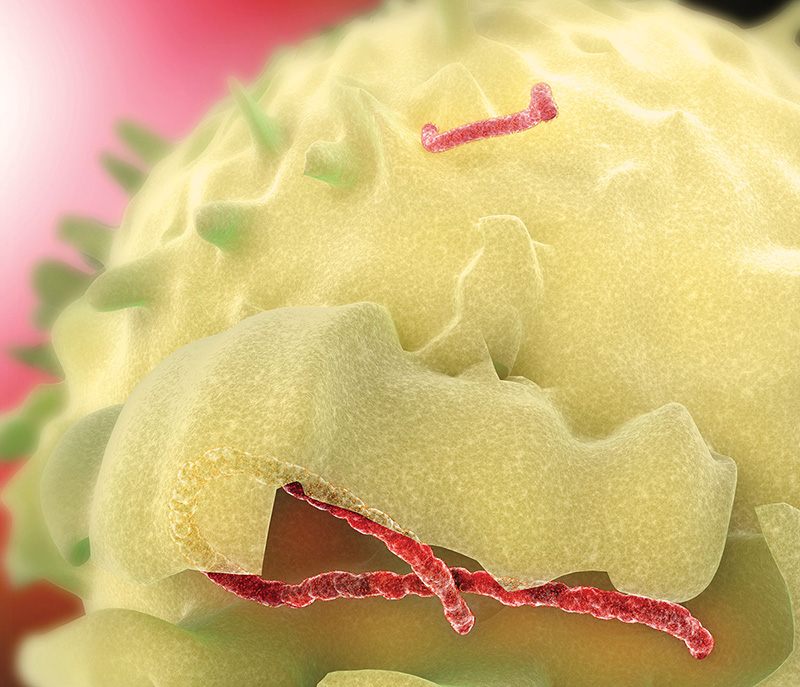
In some ways, the Ebola virus operates like a vampire; only after it is politely invited in to a host cell does it take up the task of destroying everything in its path.
The virus uses the everyday function of endocytosis—the taking in of matter by a living cell—to gain entry, first attaching to the outer wall before a vesicle forms to draw it into the cell.
In a new study supported by the National Institutes of Health, researchers at Lehigh University seek to elucidate quantitatively—for the first time—the biomechanical mechanism of Ebola-host cell interaction, providing potential new targets for antiviral drug development.
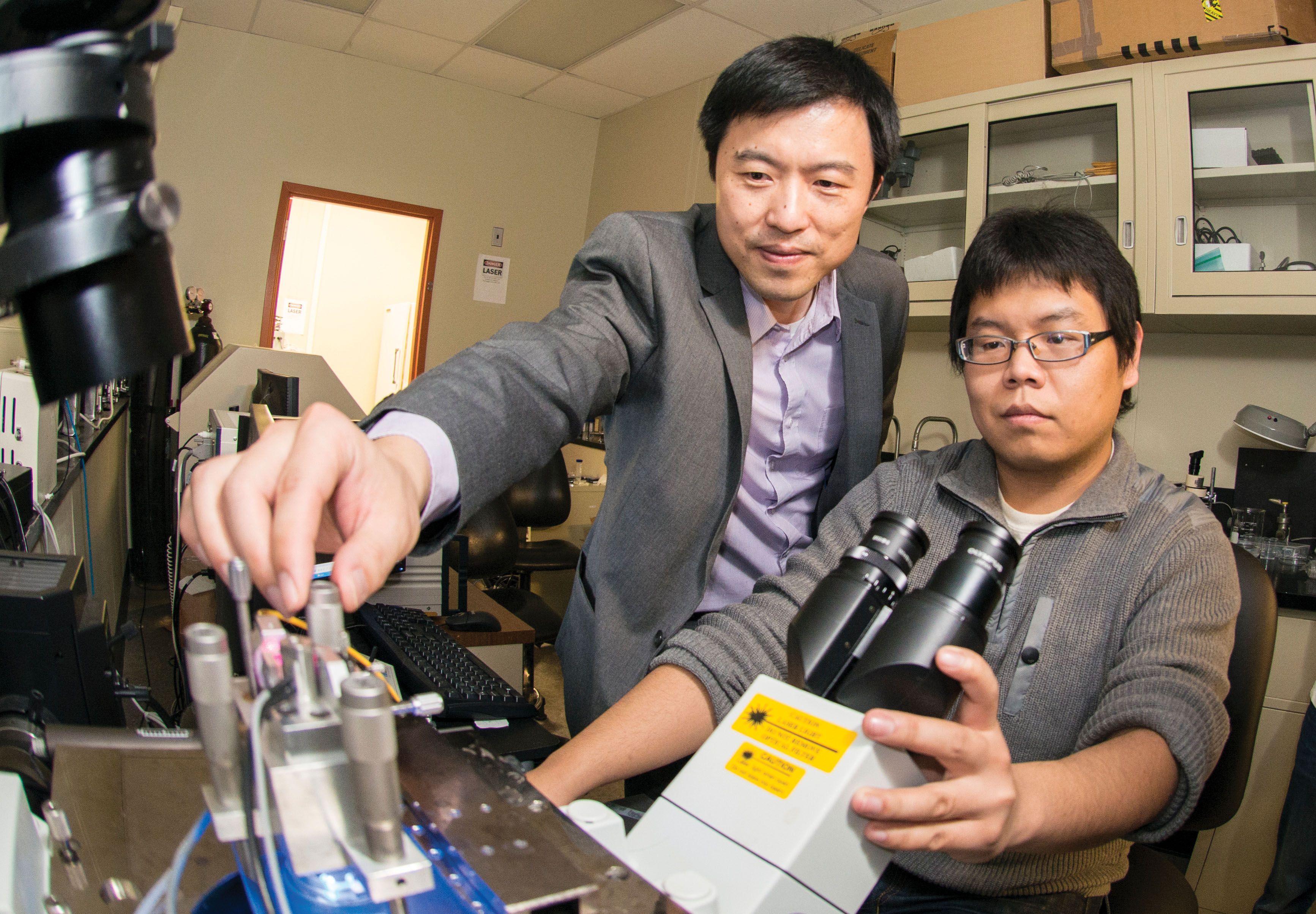
 “It is not hyperbole: the outbreak of an Ebola virus epidemic poses a major threat to the entire world,” says Frank Zhang, assistant professor of bioengineering and of mechanical engineering and principal investigator on the project. “Yet, because the mechanisms of the actual infection process remain obscure, there is still no specific treatment or vaccine for this dreaded disease.”
“It is not hyperbole: the outbreak of an Ebola virus epidemic poses a major threat to the entire world,” says Frank Zhang, assistant professor of bioengineering and of mechanical engineering and principal investigator on the project. “Yet, because the mechanisms of the actual infection process remain obscure, there is still no specific treatment or vaccine for this dreaded disease.”
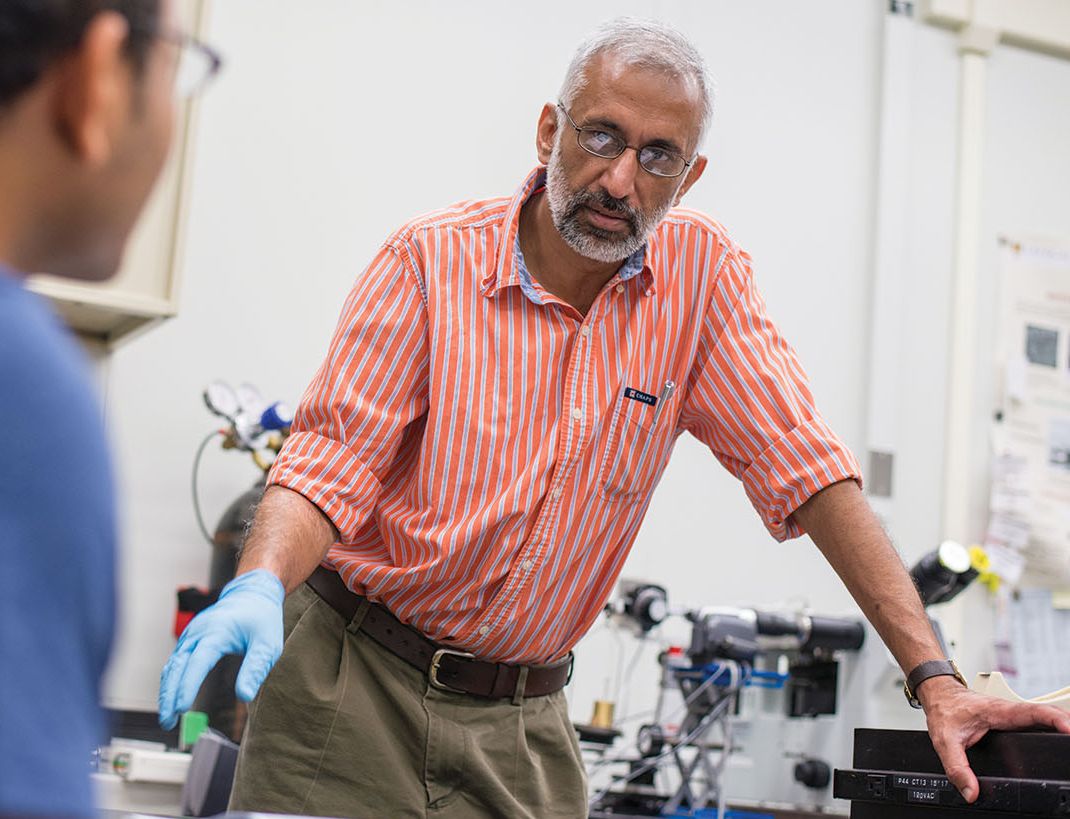
While Ebola-host cell attachment has been shown to depend on the molecular biomechanics of interaction between receptors on the cell surface and the outer coat of the virus, the quantitative understanding essential for guiding the development of therapies has yet to be developed, says Anand Jagota, co-PI on the project, founding chair of the Department of Bioengineering and Professor of Chemical and Biomolecular Engineering.
The Lehigh team supporting the project, Biomechanics of TIM protein-mediated Ebola virus-host cell adhesion, pairs Jagota’s expertise in computational molecular adhesion mechanics with Zhang’s focus in mechanosensing—how cells sense and respond to mechanical stimuli. The project, supported by the National Institute of Allergy and Infectious Diseases through a grant totaling nearly a half million dollars over a three year period, formally launched in January of 2018.
According to the team, recent work by other researchers has established the importance of the T-cell immunoglobulin and mucin (TIM) family of proteins in the virus’ ability to attach to a cell, specifically the geometry and mechanical properties of TIM’s so-called mucin-like stalk domains (MLD). Jagota and Zhang intend to use their skills in experimental and theoretical molecular biomechanics to build upon these recent findings.
“Our hypothesis is that quantitative knowledge about the length, rigidity and charge of MLD can be used to predict conditions for Ebola’s attachment,” says Jagota. “Through this study, we hope to provide new pharmacological targets and aid in the development of much-needed antiviral therapeutics for the prevention and treatment of Ebola.”