Bioengineering researcher Anand Ramamurthi leads a team developing minimally invasive techniques that could transform the treatment of aortic aneurysms
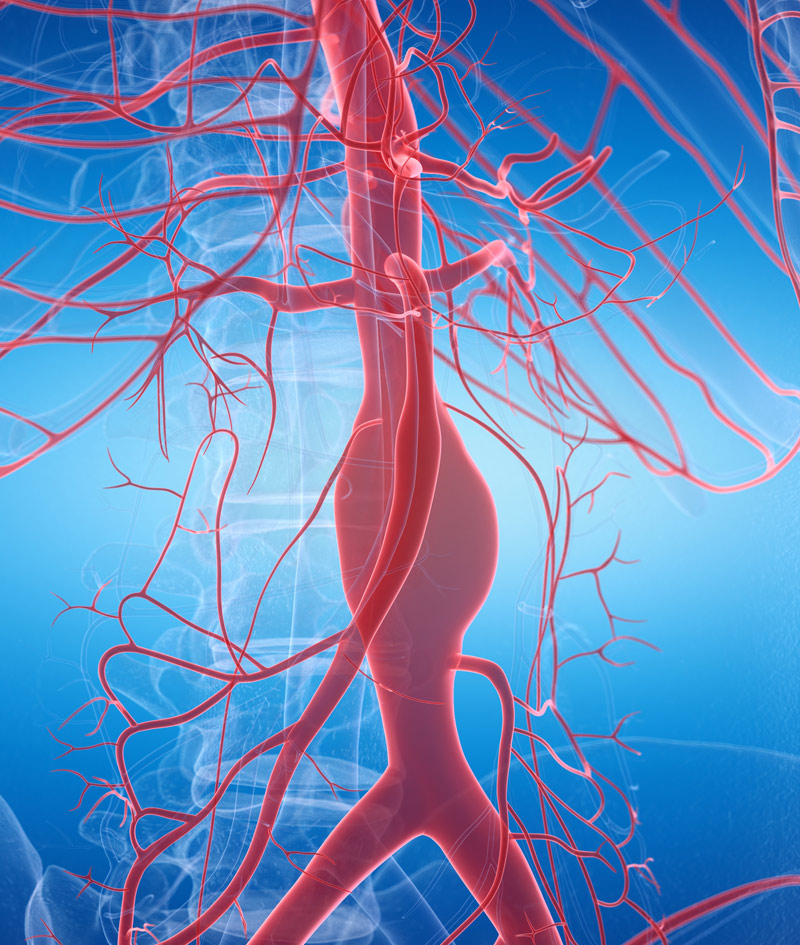 Aortic aneurysms are bulges in the aorta, the largest blood vessel that carries oxygen-rich blood from the heart to the rest of the body. Smoking, high blood pressure, diabetes, or injury can all increase the risk of aneurysms, which tend to occur more often in Caucasian male smokers over the age of 65.
Aortic aneurysms are bulges in the aorta, the largest blood vessel that carries oxygen-rich blood from the heart to the rest of the body. Smoking, high blood pressure, diabetes, or injury can all increase the risk of aneurysms, which tend to occur more often in Caucasian male smokers over the age of 65.
“The soft tissues that make up blood vessels act essentially like rubber bands, and it’s the elastic fibers within these tissues that allow them to stretch and snap back,” says Professor Anand Ramamurthi, chair of the Department of Bioengineering. “These fibers are produced primarily before and just after birth. After that, they don’t regenerate or undergo natural repair after injury. So when they become injured or diseased, the tissue weakens and causes an aneurysm, which can grow over time. After about seven to 10 years, it typically reaches the rupture stage.”
During that period, there is no treatment. Patients are screened regularly via imaging to monitor the rate of the aneurysm’s growth. Once it’s deemed big enough to potentially rupture (rupture of aneurysms is often fatal), surgery is the only option. But it’s a risky one for elderly patients.
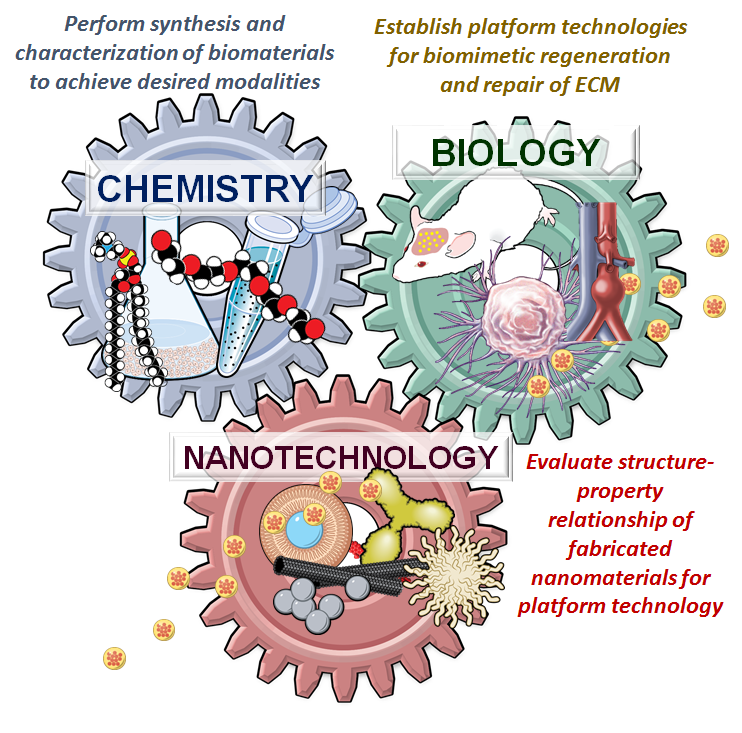
Ramamurthi and his team are working on minimally invasive ways to regenerate and repair these elastic fibers using polymeric or biological nanocapsules, called nanoparticles, that are designed to release novel regenerative therapeutics. Their innovative techniques could enable treatment soon after an aneurysm is detected and potentially slow, reverse, or even stop its growth. Findings in a paper published earlier this year in the Journal of Biomedical Materials Research build on their earlier work and represent a step toward a future where surgery is no longer the best, and only, treatment option.
“In previous research, we’ve identified drugs and gene-silencing agents that can actually coax adult diseased vascular cells to produce new elastic fibers and inhibit the enzymes that break down existing fibers,” he says. “We’ve also been working on how to deliver these therapeutics efficiently only at the site of tissue repair.”
The team has also developed a nanoparticle design called active-targeting that incorporates small protein fragments, or peptides, on the nanoparticle’s surface. “These peptides recognize components that are unique to the aneurysm tissue. So when the nanoparticles are injected into the bloodstream, they stick only to the aneurysm wall, where they slowly degrade and release the drug.
For this paper, he says, the researchers “investigated how the nanoparticles actually penetrate the blood vessel wall to deliver the drug to the affected tissue.”
All blood vessels are lined with a protective barrier made of endothelial cells, which can become “leaky” as inflammation from tissue damage or disease breaks down the endothelium and creates gaps between the cells. These gaps allow white blood cells to move in and start the tissue repair process, and they also serve as the entry point for nanoparticles that accelerate healing.
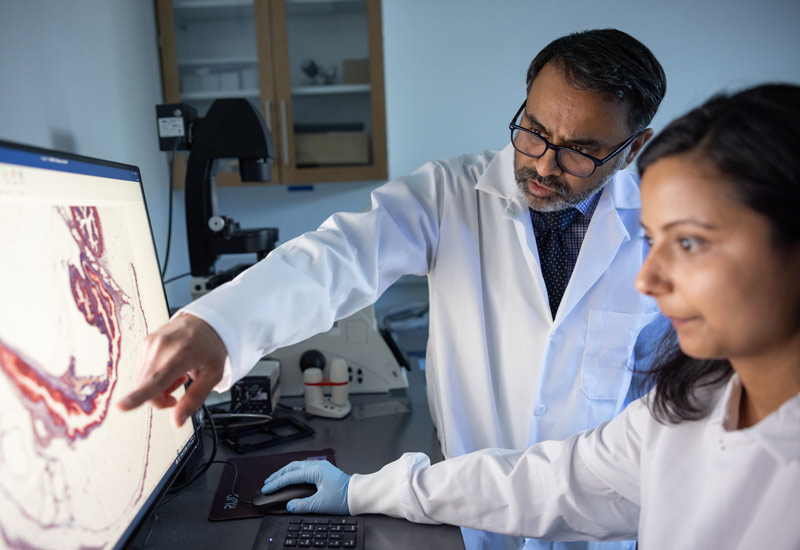 “We wanted to know how the shape and the aspect ratio of these nanoparticles affect their ability to cross that endothelial cell barrier,” says Ramamurthi.
“We wanted to know how the shape and the aspect ratio of these nanoparticles affect their ability to cross that endothelial cell barrier,” says Ramamurthi.
It was a critical question to answer because not all nanoparticles are created alike, and if they can’t penetrate the barrier, they can’t repair the tissue.
Ramamurthi and his team developed a novel cell culture model in which they simulated disease and then examined mechanisms of transport: specifically, how nanoparticles of different kinds interacted with endothelial cells and moved through them. Did they enter through gaps among the endothelial cells (a process called extravasation) or through the cells themselves (what’s known as translocation)?
“Let’s say a nanoparticle goes through an endothelial cell. Some of it might stay within that cell and not come out the other side, which means you lose that particle, and it’s no longer useful to the healing process. The goal is transportation with minimal retention.”
The team found that rod-shaped particles, as opposed to spherical particles, with a high aspect ratio (i.e., long and skinny versus short and stubby) were selectively taken up by diseased endothelial cells. “And they showed very little uptake into healthy endothelial cells compared with the spheres, which is good because we don’t want them interacting with healthy vessel walls,” he says.
They also found that particles reached the tissue primarily by extravasation (or via the cell gaps). “The longer and skinnier they were, the less likely they were to remain within the endothelial cell layer, which means they’re getting through to the affected tissue for more effective therapy.”
The team will now integrate these findings with their work on active targeting—incorporating components on the surface of nanoparticles that recognize proteins expressed by diseased cells—in animal models.
The ultimate goal is to develop a nonsurgical regenerative therapy capable of slowing aneurysm growth. For example, increasing the current growth-to-rupture stage from seven years to 15 years. An even more ambitious outcome, says Ramamurthi, would be to revert that growth.
“Regression of aneurysm growth would be the preferred long-term outcome,” he says. “That’s a long way off, but we’re excited because these findings will help guide us on how to design our nanoparticles for more efficient delivery to the aneurysm wall. It’s an opportunity to get closer to that reality.”