
By Christine Fennessy
It’s a value proposition of sorts. A promise to create meaningful change, to make a difference. For Lehigh faculty, and for students especially, that promise means that Lehigh will provide them with a foundation to make lasting—and potentially far-reaching—contributions.
“Students have fundamentally changed from when I was a student walking these halls,” says Hannah Dailey ’02, ’06G, ’09 PhD, now an assistant professor in the Department of Mechanical Engineering and Mechanics. “Engineers today are motivated by the idea of applying their engineering skills to doing good for others, for society, for the world as a whole. And one very significant way they can do that is through health and health care.”
And now, with the announcement of Lehigh’s new College of Health, there will be even more opportunity for impact through research that is devoted to making health care more accessible, affordable, and effective—collaboration that will serve to amplify research currently being conducted across the Rossin College.
A common denominator
The College of Health will begin enrolling students in Fall 2020, and will focus on population health and health data analytics. According to its inaugural dean, Whitney P. Witt, such focus will enable Lehigh to understand, preserve, and improve the health and well-being of populations and communities through excellence and innovation in education, research, and service. (See “The Power of Population Health.”)
In the lab, Dailey and her students and collaborators research computational and experimental biomechanics of fracture fixation and bone healing, fracture nonunion, and the mechanics of tissues and biomaterials. Their work toward alleviating orthopedic trauma has them partnering closely with surgeons from St. Luke’s University Health Network. She sees a clear intersection between her work and the mission of the new college.
“Anything that makes it easier to partner with the medical community to help care for patients, to bring engineering tools and methodologies to bear on the problems doctors and other allied health professionals face, is a good thing,” she says. “We will be stronger and more productive as a learning community.”
Because the problems—and hence, the possible solutions—in health care are so complex, partnerships and collaborations are the common denominator when it comes to successful innovation, says Xuanhong Cheng, an associate professor of bioengineering and of materials science and engineering.
“Take a glucose sensor, for example,” says Cheng. “For something like that, you need to interface between the biological and the abiological systems. And that requires people with backgrounds in chemistry, biochemistry, chemical engineering, and bioengineering. The instrument itself requires electrical engineering and mechanical engineering. Data is being collected in analog form, and so you need people with backgrounds in computer science who can convert the analog data to digital.”
 Another good example, Cheng notes, is the smart watch: “It doesn’t directly measure heart rate, it measures an optical signal that has to be translated into heart rate. Someone with computer science knowledge has to be able to process the data and connect it.
Another good example, Cheng notes, is the smart watch: “It doesn’t directly measure heart rate, it measures an optical signal that has to be translated into heart rate. Someone with computer science knowledge has to be able to process the data and connect it.
“And if you’re talking about collecting population data,” she continues, “those data often need to be transmitted long distance, which requires people with experience in computer science and even mathematics. So, bottom line, the development of new technology that successfully impacts health care requires input from people with a broad array of backgrounds and expertise.”
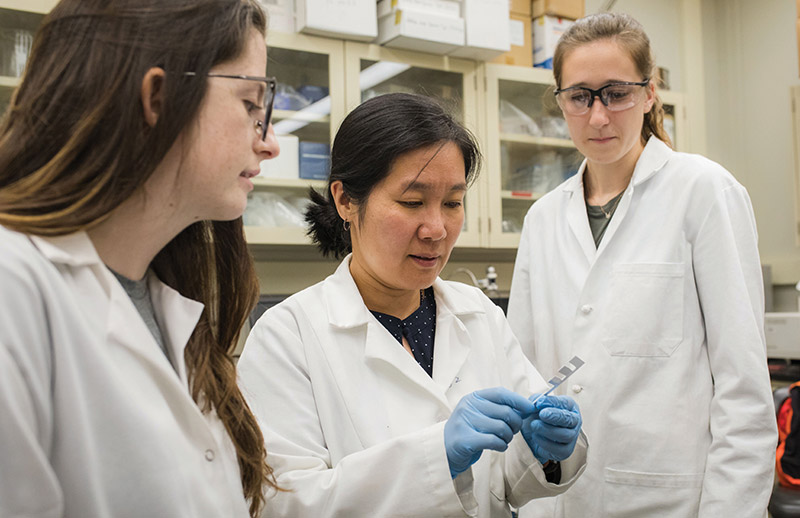
Cheng’s own research is defined by such multidisciplinary collaborations and focuses on diagnostic and therapeutic devices on the microscale. One such project is a microelectrical sensor she’s developing with James Hwang, a professor of electrical and computer engineering.
“I’m trained in the design and fabrication of small devices and how to incorporate biological samples, which means I don’t have the background or expertise that Jim has to design sophisticated electrical sensors. But together, we’re working to create a less expensive cancer diagnostic device. Basically, single-cell electrical detectors that can detect cancer cells.”
Cheng is also working with Alparslan Oztekin, a professor of mechanical engineering and mechanics, and James Gilchrist, a professor of chemical and biomolecular engineering, on a microfluidic device that can detect infection. “We’re looking at using the device for analyte separation, separating pathogens from bodily fluid,” she says. “This particular project requires a lot of transport knowledge and experts in transport phenomena.”
With Filbert Bartoli, a professor of electrical and computer engineering, she’s developing optical sensors that can monitor immune function, and with Frank Zhang, an associate professor of bioengineering and mechanical engineering and mechanics, sensors that can detect and rectify mechanical stress within the body.
Cheng also mentors a student-led project that is developing point-of-care diagnostics for sickle cell disease and anemia to be used specifically in Sierra Leone. The project is part of the Global Social Impact Fellowship, a program for undergraduate and graduate students from all disciplines across the university that integrates experiential learning, research, and entrepreneurial engagement.
“There are just so many components involved in health-related problems, that I think it’s natural to have these interdisciplinary connections,” she says.
Such a collaborative ethos will no doubt characterize the College of Health. To dovetail with the college’s focus on population health, Cheng says the Department of Bioengineering will launch a biocomputation program this fall. (See “A Major Development.")
“Studying population health means collecting data on a large scale, which requires developing hardware and training students in biocomputational skills,” says Cheng. “This program will teach them health data analytics and how to analyze biophysical data. So the overlap between the new program and the new college is significant.”
Breaking boundaries
For Kelly Schultz, the interdisciplinary mindset is key to the continued progress at Lehigh toward the ultimate goal of making health care more accessible, affordable, and effective.
“When it comes to the kind of research that I do, it’s quite important,” says Schultz, who is an associate professor of chemical and biomolecular engineering. “We’ve been doing work on changing the enzyme secretions of cells, and I’m not a biologist. Without help from Susan Perry [who is a professor of practice in bioengineering] I wouldn’t have known how to go about designing those experiments.”
Schultz, Dailey, and Cheng are also affiliated with the Institute for Functional Materials and Devices, one of Lehigh’s three Interdisciplinary Research Institutes. I-FMD assembles expertise from across the university in the synthesis, fabrication, processing, and characterization of engineered materials including semiconductors, metals, ceramics, composites, polymers, and other soft materials. I-FMD has several thrust areas, and Schultz and Dailey are part of a team looking at advancing the science of wound healing. (Cheng’s team is looking at soft, active materials.)
“There are people in the group from bioengineering, chemistry, mechanical engineering, materials science,” says Schultz. “We bring our interests in health and wound healing to the table, and some really interesting and creative ideas have come out of those meetings, ideas we wouldn’t have considered on our own as individuals.”
Schultz’s interest in helping people live longer, healthier lives is largely driven by a fascination with just how well the body does on its own.
“Our bodies are already pretty efficient,” she says. “People are starting to live into their hundreds now, and not just because of technological interventions. Some people just live longer and their bodies do better. So why reinvent the wheel? Why not take what already works and then try to make it somewhat better? If it’s possible to live a long time with very little intervention, we can take inspiration from those people and use it to help the person who has a very bad diagnosis and a short life expectancy.”
To that end, Schultz’s lab is trying to ramp up the body’s wound-healing ability. She’s working on implantable materials called hydrogels that contain stem cells, which naturally temper inflammation.
“Wounds can go chronic if there’s too much inflammation, and stem cells can stop that inflammation,” she says. “They do that by restarting the healing process, calling the right cells to the wound to form tissue, and changing into different cells to regenerate tissue. So what we want to know is, how can we get more of these good cells to the wound and how can we get them there faster?”
Schultz’s lab is laying fundamental groundwork as they seek to reveal how cells move within the hydrogel and how that movement can be directed. The potential applications for the hydrogels could be especially profound for burn patients and people dealing with diabetes complications, both of whom experience the debilitating pain of chronic wounds.
Outside of wound healing, Schultz and her team are also looking at materials that can enhance drug delivery, specifically in the gastrointestinal tract. Nutrients and drugs are generally absorbed in the intestines, but the stomach’s high acidity can often neutralize the active molecules that provide the nutrition, or the relief. Schultz is working with an inexpensive, more versatile coating that can protect those molecules.
Schultz pauses when considering the potential reach of her work. Hers is building-block research. The kind of work that answers the fundamental questions of why and how a material works, so it can be better manipulated to improve health. “So I don’t see myself developing a new treatment that would be delivered directly to patients,” she says. “My work will hopefully support the efforts of other researchers developing such treatments.”
What she has done—and continues to do—is step outside the boundaries of her discipline and consider the types of questions and solutions that aren’t typical in her scientific community of rheology, the study of the deformation and flow phenomena of materials.
“In my core area, there isn’t much focus on biological questions, but we could answer a lot of them. I’d like to see more people in the rheology community looking at biological problems and more people in the biomaterials community listening to what rheology has to say—a more interdisciplinary approach,” she says. “There are only a few of us who collaborate across those communities, and there are just so many questions and they’re so interesting. I’ve been trying to push to get both communities to listen to each other, broaden our areas of research, and complement each other’s work.”

She says the College of Health will offer yet another perspective on those interesting questions.
“The new college will provide us with much more depth around some of the social issues that we don’t currently consider,” says Schultz. “And that will keep us all moving in the right direction towards helping people live better lives.”
Impact through innovation
It’s an exciting time for an engineer at Lehigh to make her mark on health care and improve—via devices, materials, software, hardware—the well-being of society.
“The investment Lehigh is making in the College of Health reflects a long-term vision for impact through innovation,” says Dailey. “There will be even more opportunity for educational experiences and meaningful contributions in health care. And that is well aligned with students’ values. The added visibility of the new college will help students recognize that they can do good in the world through innovating better health care technologies and medical devices and partnering in really meaningful ways. I think that’s going to be inspiring to this generation.”
It’s the kind of inspiration that continues to drive Dailey, whose research interests include bone fractures, bone fracture healing, and bone mechanics. Specifically, her lab uses CT scans to model the properties of bones and how they heal after a fracture, and they do numerical modeling to predict how mechanical forces contribute to the biological response that causes those fractures to heal. Her other projects include studying the mechanics of aging bones, and combining virtual mechanical testing of CT scans with an optimization algorithm to determine the mechanical properties of callus, the spongy material that forms along a fracture line and over time hardens into new bone (see page 2).
 “I think one of the things that’s really exciting for mechanical engineers about getting into this field is that the pathway from a sketch on a whiteboard to the fruition of an idea is shorter. It’s hard to translate something from a cell model into something that can go into a human. That’s a really, really long pathway. My personal research strategy is to go at it from the other end of the pipeline. I partner with surgeons who already have patients and we pull that data backward into the engineering pipeline, instead of trying to push it forward from basic to clinical. So that’s a different strategy,” says Dailey.
“I think one of the things that’s really exciting for mechanical engineers about getting into this field is that the pathway from a sketch on a whiteboard to the fruition of an idea is shorter. It’s hard to translate something from a cell model into something that can go into a human. That’s a really, really long pathway. My personal research strategy is to go at it from the other end of the pipeline. I partner with surgeons who already have patients and we pull that data backward into the engineering pipeline, instead of trying to push it forward from basic to clinical. So that’s a different strategy,” says Dailey.
“And I think that type of strategy is pretty well aligned with where the College of Health is positioning itself. We’re not going to be developing new pharmaceuticals or blockbuster drugs, like basic science to clinical translation. We’re going to be focused on value-based health care.”
For the greater good
Impactful and valuable. Collaborative and meaningful. All words that describe the current research into improving health and health care. They also describe the promise that Lehigh is making to its future engineers. The promise that has grown even brighter as a wider range of opportunities and experiences opens up with the College of Health. The promise that they can literally change someone’s world.
“My work here can have immediate impacts on people’s health, well-being, and quality of life,” says Dailey. “I feel deeply, passionately invested in the idea that as engineers, we can contribute in a substantive, exciting way to this communal goal of better health, and we can deliver it at a lower cost. It’s why I get up in the morning. I love what I do.”


