The politics of healthcare may be impossible to predict, but one trend in medicine seems certain to gain momentum in the 21st century: Engineers working with biologists and physicians will develop new therapies, new devices and new diagnostic tools that improve the quality of life while giving people more control over their medical choices.
Indeed, says Anand Jagota, considering the potential benefits, engineers are compelled to expand the role they play in medicine.
“The huge expense of healthcare in the United States is unsustainable and is a drag on the economy,” says Jagota, a professor of chemical engineering who directs Lehigh’s bioengineering program. “This is due partly to the system and partly to tremendous inefficiencies in healthcare delivery itself.
“Engineers cannot necessarily reform the system, but we can help make the delivery of healthcare cheaper, simpler and much more efficient, and we have an obligation to try to do so.”
Jagota is taking the lead in a collaboration between Lehigh and the Mayo Clinic in Rochester, Minn., whose goal is bold if not breathtaking: To help bring about a revolution in medical care that parallels the metamorphosis of agriculture and manufacturing in the 20th century.
The research and educational partnership counts more than three dozen participants. Key players at Mayo include Gary Sieck, vice dean for research and chair of the physiology and biomedical engineering department, and Michael Yaszemski, chair of the division of spine surgery in the orthopedic surgery department. The team at Lehigh includes Mayuresh Kothare, professor of chemical engineering, and Filbert Bartoli, department chair of electrical and computer engineering.
During the last century, say the researchers, agriculture and manufacturing evolved from “diverse, small-scale and independent entities to coordinated and efficient integrated systems” producing many times more goods and services with a small fraction of the previous work force. Medical care today is ripe for a similar transformation in accessibility, affordability and efficiency – if engineering principles and technological advances are applied systematically across modern medicine’s broad and diverse landscape.
A three-pronged approach
Researchers from Lehigh and Mayo are working on projects in three categories: medical systems engineering, integrated devices and monitoring, and emerging medical materials. Advances in these areas, the researchers say, promise to have a significant impact on several aspects of future medical care.
Imagine, for example, taking cell phones and other wireless mobile gadgets and fitting them with biocompatible sensors and optical attachments that monitor the body’s vital signals as people work, play and sleep. These new devices will alert users, and the healthcare providers in a user’s network, when a trip to the hospital or clinic is in order. They will also house medical histories and records. In the process, they will decentralize medical care, says the Lehigh-Mayo team, by extending diagnosis and treatment beyond hospitals and clinics into aspects of a patient’s daily life.
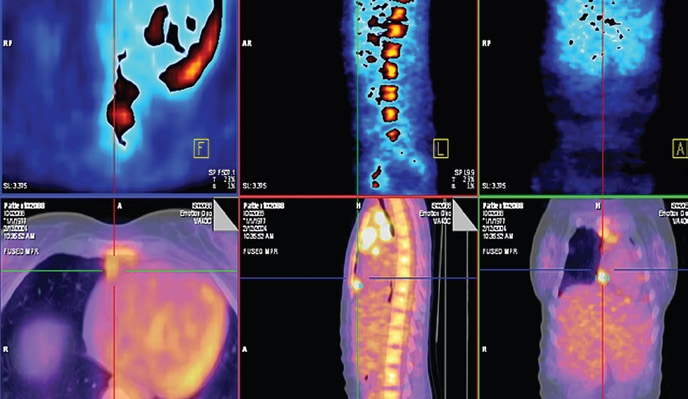
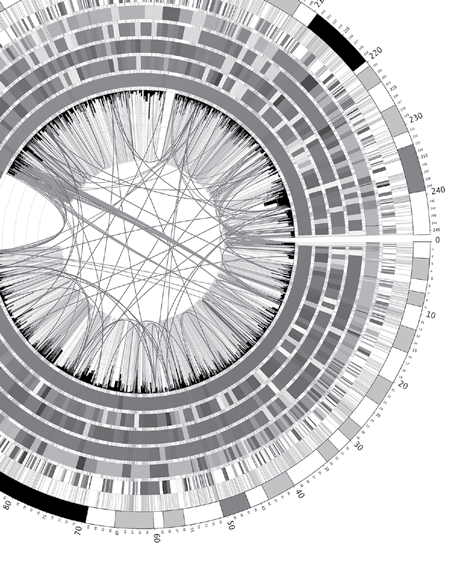
On another front, new devices and software will enable patients to “self-administer” many of the monitoring, therapeutic and drug-delivery functions that specialists now do, again cutting costs. Advances in understanding the human genome will allow doctors to personalize treatment. Microfluidic devices will enable “point-of-care” diagnoses that eliminate the need for samples to be sent to labs. Intuition born of professional experience will still be critical, but more and more medical decisions will be assisted by precise measurements interpreted by computers that learn from vast medical information databases.
Simplification, automation and miniaturization, say the researchers, will result in devices that cut costs by allowing expensive medical procedures to be moved away from specialized facilities requiring highly trained operators to doctors’ offices and eventually to home care.
Meanwhile, new materials will lend greater biocompatibility to artificial organs and synthetic tissue. Coupled with advances in bioelectronics and biophotonics, for example, a new generation of microchips could be developed that, when implanted in the brain or spinal column, will rewire nerve cells, rejoin synapses and reconnect nerve signals to muscles. Similarly, implanted microdevices will achieve “as-needed drug delivery” by, for example, triggering a surge of insulin when glucose levels rise.
Critical to all three of these areas, say the Lehigh-Mayo researchers, and critical to the overall drive to make medical care more affordable with technology, is systems engineering. “In the future healthcare system,” the researchers believe, “constant monitoring of patients will produce vast data sets for new clinical research studies. It will enable early identification of the onset of disease and greater quality and duration of life outside managed-care facilities.
“Many innovations will be required, such as novel, unobtrusive sensors; power-efficient, small-form-factor data-acquisition, storage, and analysis units; and power-efficient, high-reliability, high-availability, secure communications and networking solutions. This wealth of challenges opens exciting new opportunities for students in engineering and students in medicine.”
The new partnership thus has an important educational component: Mayo students seeking the Ph.D. or M.D. in biomedical engineering will study at Lehigh to master engineering fundamentals and quantitative systems skills, while students in Lehigh’s new bioengineering Ph.D. program (see page 23) will complete laboratory rotations or clinical internships at Mayo. These exchanges will give students an integrated biomedical and systems engineering perspective and enable them to develop the “essential technology framework for affordable medical care.”
The Lehigh-Mayo collaboration is a key element of the emerging Lehigh Biotech Cluster, a comprehensive initiative designed to support the efforts of biomedical researchers and leverage capabilities in advanced materials, optical technologies and systems engineering.
A logical merging of interests
The Mayo Clinic enjoys renown not only for the quality of medical care it delivers but also for its efforts to reduce the cost of its services. President Barack Obama has praised Mayo for offering “the best quality and lowest cost of just about any healthcare system in the country” and has urged other providers to “learn from what Mayo is doing.” Journalists and bloggers have joined the National Academy of Engineering in lauding Mayo’s commitments to “patient-first medicine” and “team medicine.”
Lehigh in recent years has forged research partnerships with hospitals, medical schools, and medical technology and drug companies. These include the Johns Hopkins University School of Medicine, the Lehigh Valley Hospital, Merck and Co. Inc., Olympus, B. Braun, and Becton, Dickinson and Co. (BD). In 2002, with support from NSF, Lehigh launched an undergraduate bioengineering program (see page 22) with concentrations in cell and tissue engineering, biopharmaceuticals, and bioelectronics/ photonics.
In 2007, to coordinate research efforts in diagnostic and therapeutic technologies for affordable medicine, Lehigh’s board of trustees approved the Biotech Cluster. The endeavor is part of the university’s Healthcare Initiative, which is a centerpiece of Lehigh’s 10-year strategic plan. A specific plan has been developed to establish a state-of-the-art facility to house the Biotech Cluster and create space for Lehigh’s biomedical researchers and for collaborative projects with Mayo. The initiative also calls for a major expansion of the bioengineering faculty, the appointment of endowed chairs in health and the construction of user facilities devoted to cell-tissue cultures, imaging and characterization, device microfabrication, and genomics and proteomics.
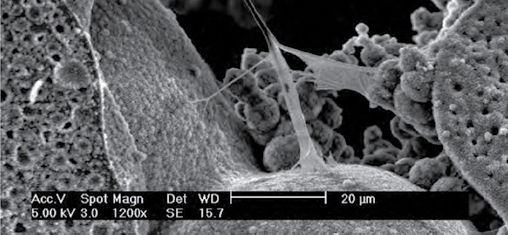
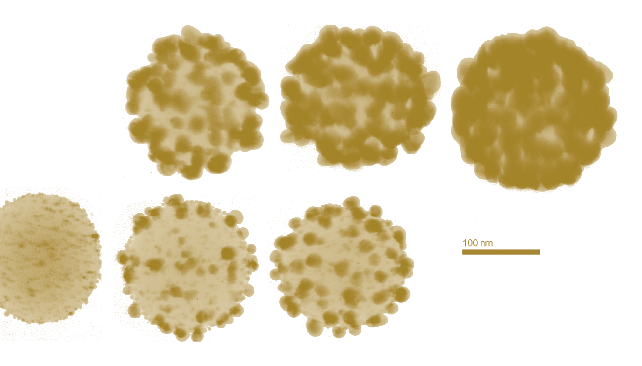
Lehigh’s areas of expertise are well-suited to the needs of advanced biomedical research. The university’s spectroscopy and microscopy facilities are world-renowned for their ability to characterize the properties and behaviors of materials at the nanoscale. The newly restructured Emulsion Polymers Institute has first-class labs for synthesizing and characterizing polymers and colloids. The Center for Optical Technologies and Sherman Fairchild Center for Solid-State Studies contain labs that are ideal for the fabrication of microelectronic devices capable of sensing and manipulating cells, molecules and nanoparticles.
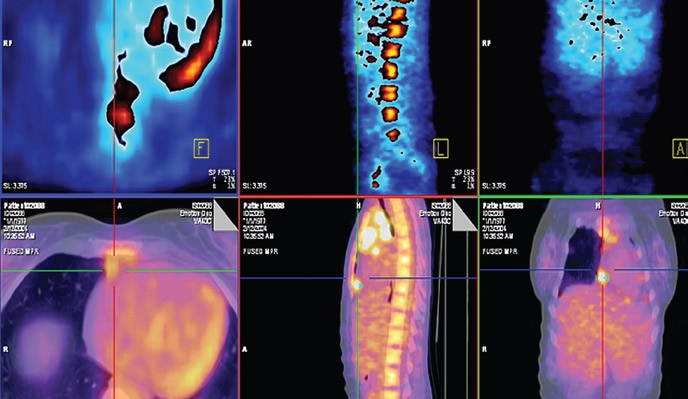
Biomedical research efforts now underway at Lehigh and at Mayo are highly complementary. At Lehigh, computer scientists are automating the analysis of MRIs and other medical images with novel computational and data-processing tools. Chemical engineers are developing nanomaterial hybrids of DNA with carbon nanotubes, while chemists are sequencing single DNA molecules with magnetic “tweezers” using massively parallel dynamic force spectroscopy. Electrical engineers are applying bioMEMS (microelectromechanical systems) to study lung cells and, separately, developing arrays of microelectrodes to monitor electrical activity in neuronal networks. Physicists use laser “tweezers” to manipulate and study cells, and materials scientists and mechanical engineers are learning to control the differentiation of adult stem cells.
At Mayo, a team of biomedical engineers is developing wearable monitors to gather patient data for studies in endocrinology and obesity, as well as orthopedics and neurology. Wireless devices communicating with the monitors will process data and transfer it to an upstream network. The project requires solving, and integrating, issues related to the flow and analysis of information, the reliability of data, the detection of anomalies, and the privacy and security of data traversing through a network. The Mayo group is collaborating with an electrical engineer at Lehigh (see page 2) who has expertise in wireless communications networks.
Ubiquitous, 24/7 care
Solving challenges like these, say the Lehigh-Mayo researchers, will enable healthcare networks to reach patients in any location at any time, thus cutting costs by reducing patient travel times and hospital visits.
In one proposed collaboration, Mayo’s Sieck and Lehigh’s Kothare will investigate the implantation of chips and microdevices that could restore function to patients with Parkinson’s disease, epilepsy, cerebral palsy and other neurodegenerative conditions. The issues involved are deepbrain stimulation, brain-computer interfaces, computational modeling and control theory. Under the educational component of the Lehigh-Mayo partnership, a Mayo student would study control theory at Lehigh while a Lehigh student would learn at Mayo how to apply control theory to patients undergoing neuro-rehabilitation therapy.
In another proposed joint project, Mayo researchers are exploring vibroacoustography, an imaging method used in radiology that produces speckle-free images of tissues while offering a low-cost alternative to magnetic resonance imaging (MRI). Mechanical engineers at Lehigh will contribute expertise in large-scale numerical analysis, including finite element analysis, which clarifies the results of lab experiments by improving the characterization of the material properties of biological tissues. Finite element analysis, say the researchers, “can provide valuable insights into the mechanical response of tissues that are unobtainable by any other technique.”
The overall goal of all the LehighMayo partnership goes beyond developing new devices, systems and therapies to propose a fundamentally new approach to medical care.
“The discoveries in biology in the last half-century,” says Jagota, “have changed the way we look at the world. Now it’s incumbent on us to develop systems that can handle the complexity of biological processes and generate efficiencies.”