Medical science has not yet developed a cure or vaccination for AIDS or for the HIV virus that causes it, but efforts to combat the global AIDS epidemic appear to be having some effect.
According to UNAIDS (the Joint United Nations Program on HIV and AIDS) and the World Health Organization (WHO), the estimated number of new HIV infections reported annually has dropped 30 percent worldwide since it peaked at 3.5 million in 1996.
The number of people dying from AIDS-related diseases is also declining, the two organizations say. And new treatments are enabling persons with HIV to lead productive and, in many cases, long lives.
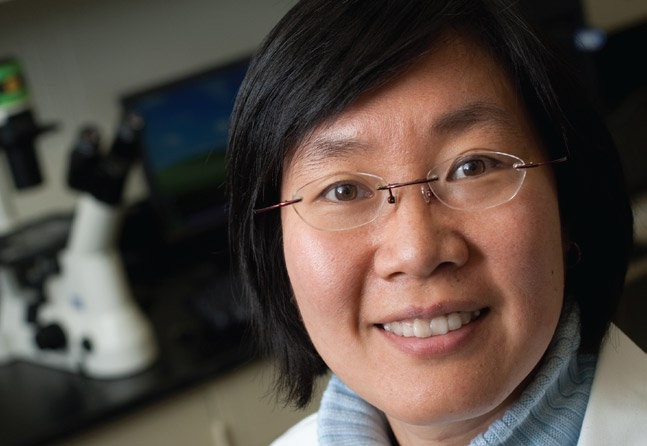
This encouraging news, says Xuanhong Cheng, is tempered by the tragedy of sub-Saharan Africa. Of the 33.4 million people in the world now coping with HIV, twothirds live in sub-Saharan Africa. And more than 14 million children in the region, according to UNAIDS, have lost one or both parents to AIDS.
For Cheng, an assistant professor of materials science and engineering, one statistic stands out. More than 400,000 children each year are infected with HIV. The vast majority contract the virus through mother-to-child transmission, a phenomenon that occurs during pregnancy, labor, childbirth or breastfeeding. Preventing or decreasing the likelihood of mother-to-child transmission is a top priority of global health organizations.
HIV testing and diagnosis are critical to this effort. But in Kenya, to cite one example, an estimated 83 percent of the people with HIV remain undiagnosed because of the lack of resources in hospitals and clinics. To help overcome the shortage of facilities and staff in outlying areas, as well as difficulties in transportation, health officials are seeking to develop point-of-care diagnostics that eliminate the need to send blood samples and other specimens to laboratories for analysis. The goal is twofold: to determine if a child is infected with HIV and to monitor the progress of the disease, thus helping a doctor decide what level or type of treatment is necessary.
Tracking the progress of HIV
Cheng is part of a research team that has developed a hand-held point-of-care diagnostic device that monitors the progression of HIV by measuring the concentration of lymphocytes – a type of white blood cell – that possess a CD4 receptor on their surface in a droplet of blood.
CD4 receptor and uses the cell to make copies of itself, completely damaging the cell in the process. Because CD4 cells help initiate the body’s response to invading microorganisms, they are a vital component of the immune system. If they are destroyed, the immune system is compromised. A CD4 count in a healthy individual is around 1,000 cells per cubic millimeter of blood. Values below this level may indicate the early stages of the disease even though the patient might not show any symptoms. Counts below 200 are a sign that the immune system has been severely weakened and the patient is then classified as having AIDS.
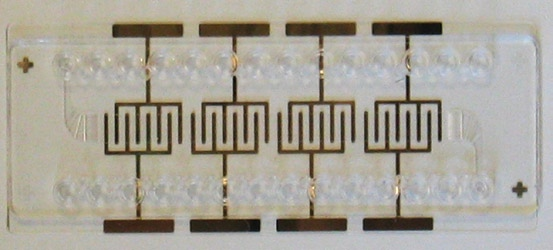
This CD4-counting device that Cheng helped develop is now being made commercially by Daktari Diagnostics Inc., a company based in Cambridge, Mass., that was founded by Bill Rodriguez, a former professor at Harvard Medical School. The device uses microfluidic cell chromatography to isolate cells from a blood sample without having to add chemical reagents. A droplet of the patient’s blood enters a tiny channel into an assay chamber whose walls contain antibodies that act like Velcro, capturing only the CD4+ lymphocytes. Everything else in the blood passes through. The chamber contains a simple electrical contact that is used to detect the number of captured cells.
A mission to Kenya
Cheng’s group is hoping to carry out a field test of the hand-held CD4-counting device later this year in Africa. In December 2009, to gain a better understanding of the conditions faced by African healthcare professionals, Cheng went on a weeklong fact-finding mission to Kenya. The trip was organized and funded by PATH, an international nonprofit organization dedicated to finding solutions to world health problems.
“To me, the use of this technology is straightforward, but there was no way of identifying potential problems without talking to Kenyan healthcare workers and seeing for myself the conditions in which they have to work,” says Cheng.
In Kenya, there are several different grades of health facility ranging from major National Referral Hospitals to local healthcare centers and dispensaries. The larger and better-equipped hospitals are situated near urban centers such as Nairobi, Mombasa, Nakuru and Kisumu. In rural areas, patients have access only to small healthcare centers, dispensaries and mobile clinics, many of which do not have a full-time resident doctor.
During the first three days of her trip, Cheng visited the Mbagathi and Kiambu District hospitals, the Karuri Health Centre, the National Public Health Laboratory and the Kenya Medical Research Institute (KEMRI) in Nairobi. On the fourth day she flew to Kisumu, a town in eastern Kenya.
“With the exception of KEMRI, laboratory facilities in Kenya are minimal, even in the large hospitals,” says Cheng. “A lab is considered to be well-equipped if it has a microscope and a centrifuge. A major problem is that all the samples obtained from patients throughout the hospital, irrespective of the disease, are analyzed in the same room. Ventilation is often inadequate. This can lead to cross-contamination and to the spread of disease to the people who work there.”
In addition, a stable electricity supply cannot be guaranteed and power, in many cases, is available only during the day. And the lack of air conditioning means that temperatures inside hospitals vary considerably from day to night. “This has serious implications for the use of our device as we use electrical measurements to obtain a CD4 cell count,” says Cheng. “We may now have to introduce a selfcalibrating system into our device so that it can be operated at different temperatures.”
Funding for healthcare systems in Kenya has not increased for several years and hospitals are lucky if they have 60 percent of the required staff. Money for even the most basic of diagnostic testing is limited. All funding for point-of-care diagnostics would have to be obtained from outside charitable agencies.
An affordable blood test for HIV
Despite these challenges, says Cheng, the healthcare workers she met were dedicated, often working long hours.
“One thing you notice is that the Kenyan people in general are always smiling,” she says. “They seemed very pleased to see us and waved to us as our cars went by. The visit has made me even more determined to play a part in improving their level of health care.”
Back at Lehigh, Cheng is working on a second hand-held point-of-care diagnostic device that will measure the concentration of HIV virus particles present in a blood sample.
“HIV diagnosis in adults is simple,” says Cheng. “You take a sample of blood or saliva and put it on a strip. If the blood contains HIV antibodies, the strip changes color and you know the patient is infected with the virus. Diagnosis in infants, however, is not as straightforward. A baby receives a lot of antibodies from its mother so the only way to confirm whether or not a baby has HIV is to detect the number of virus particles in the blood.”
Currently, HIV viral loadings are measured using one of three proprietary commercial methods. All are based on nucleic acid amplification and all require state-of-the-art laboratory facilities that are prohibitively expensive and not available in developing countries.
Cheng’s second hand-held device, also based on microfluidic technology, will be more complicated than the CD4- counting device because HIV viruses are much smaller than CD4 cells and therefore more difficult to detect.
The new device will contain a prefiltration chamber designed to separate out viral particles, which are only 120 nm in diameter, from much larger particles such as red and white blood cells. The amount of blood required for this test is approximately 1 milliliter – considerably more than the single droplet required for the CD4- counting device. By passing this larger quantity of blood through the chamber, the concentration of viral particles is increased 1,000 times, which makes them easier to detect and leads to a more accurate measurement of concentration. The separated viral particles will then be impregnated into a nanoporous membrane that contains specific antibodies to which the viral particles will selectively adhere. The number of particles will be determined from the pressure differential across the membrane.
Designing this type of device requires expertise in several fields of materials engineering and biomedical science. Cheng is collaborating with Profs. Wojciech Misiolek and William Van Geertruyden of Lehigh’s materials science and engineering department and with Dr. Timothy Friel, an infectious disease specialist at Lehigh Valley Hospital in Allentown, Pa. Daniel Ou-Yang, a professor of physics, is helping Cheng determine the feasibility of using optical techniques to measure viral concentrations.
“While both of these devices are designed for point-of-care diagnostics in developing countries, there is no reason why they can’t be used in the U.S.,” says Cheng. HIV patients are advised to check their viral loading every four months to monitor the effectiveness of their treatment regime. Cheng’s devices could lead to a more cost-effective and accessible method of monitoring the disease.