A heart attack can cause extensive scarring of the cardiac muscle tissue, which the damaged tissue itself cannot repair. In an attempt to maintain a viable cardiac output, the walls of the heart narrow and the left ventricle dilates to increase stroke volume. Often this structural remodeling is not sufficient to restore normal blood flow and leads to congestive heart failure, the number one cause of death in the U.S.
A heart transplant is the ultimate solution, but a lack of donors and complications from immune-suppressive treatments have spurred scientists to seek new strategies to regenerate injured heart tissue.
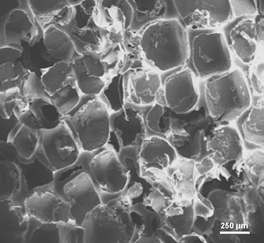
One promising approach is to implant a cardiac patch composed of heart muscle cells, or cardiomyocytes, grown on a porous polymer scaffold.
“The scaffold provides mechanical support for the cardiomyocytes,” says Sabrina Jedlicka, an assistant professor of materials science and engineering, “and facilitates their integration into existing tissue.”
Many researchers have built scaffolds from conventional biomaterials like Dacron. Jedlicka and Courtney LeBlon, a graduate student, are evaluating scaffolds made of biodegradable polymers whose elastomeric properties mimic those of living heart muscle tissue.
“The scaffold with an elastic modulus closest to that of healthy heart muscle is made of polyglycerol-sebacate (PGS),” says Jedlicka. “The chemical nature of this polymer, specifically its hydroxyl component, could also provide an ideal surface for the adhesion of cardiomyocytes.”
Jedlicka and LeBlon seeded the new porous scaffold with cardiomyocyte cells from mouse embryonal P19 carcinoma cells to see if the cells would thrive on the platform. P19 cells can be transformed into cardiomyocytes by exposing them to dimethyl sulfoxide using a “hanging drop” technique.
The researchers placed one droplet of P19 cells onto each side of the PGS scaffold and incubated them for 14 days. The P19 cells were transformed into cardiomyocyte-like cells with a contractile ability that was assessed every two days by taking voltage readings.
“While scaffolds made from other materials did support some level of cell contraction, PGS was by far the best,” says LeBlon. “This is primarily because its mechanical properties are comparable to those of healthy heart muscle tissue.”
“The only problem is that the cardiomyocytes on our current scaffolds are beating out of step,” says Jedlicka. “We are trying to modify the scaffold to induce a more uniform alignment of the cells that will hopefully lead to synchronous contraction.”